Why Remote Patient Monitoring is Changing Healthcare
Remote patient monitoring (RPM) allows patients to collect their own health data—like blood pressure, weight, and glucose levels—using connected medical devices that automatically transmit information to their healthcare providers. Instead of waiting for your next appointment to share how you’re doing, RPM gives your care team real-time visibility into your health, enabling them to intervene early when problems arise.
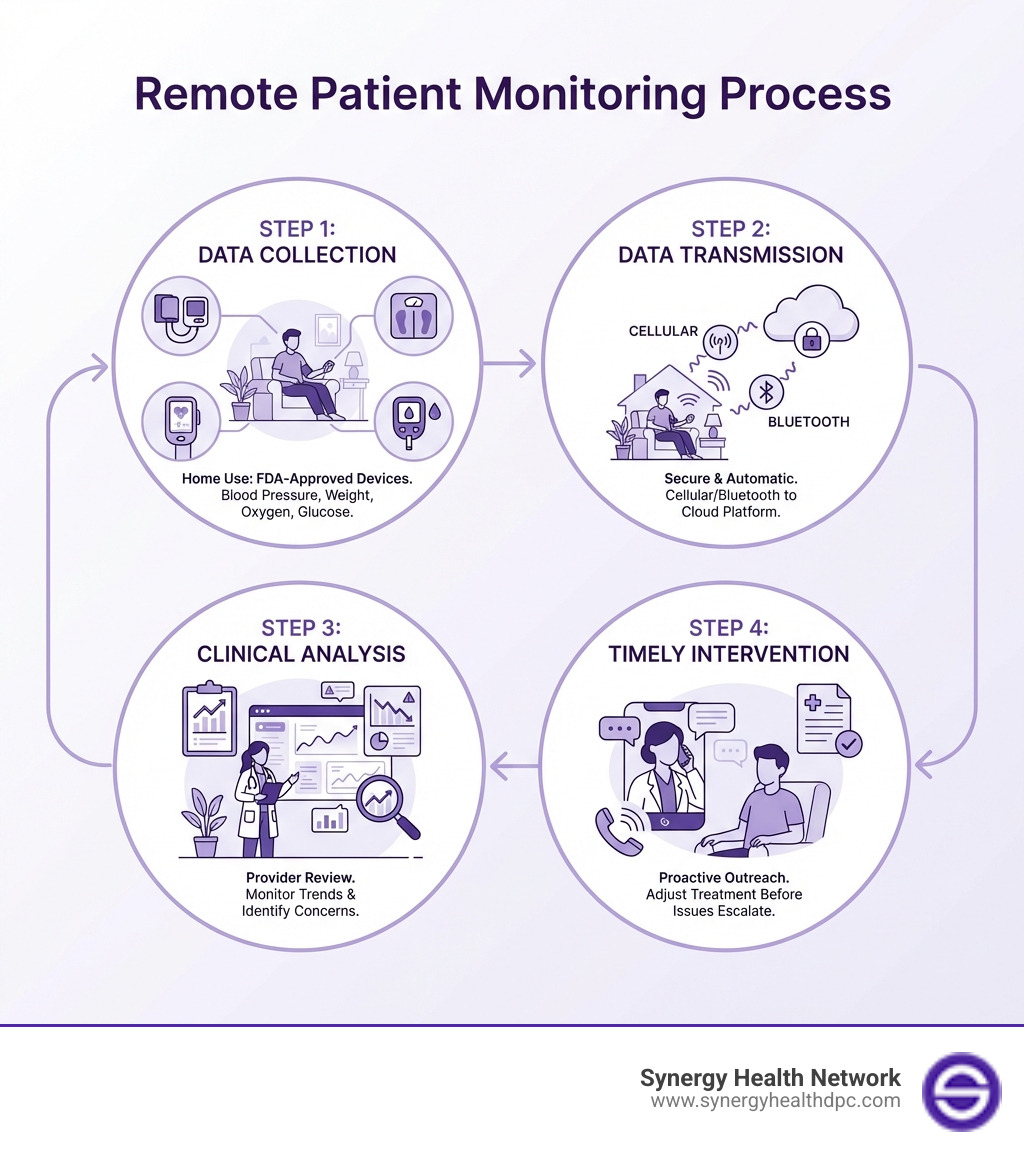
Here’s how Remote Patient Monitoring works:
- Data Collection – You use FDA-approved medical devices at home (blood pressure cuff, scale, pulse oximeter, glucose meter)
- Data Transmission – Your readings automatically upload to a secure platform via cellular or Bluetooth connection
- Clinical Review – Healthcare providers monitor your data and identify concerning trends
- Timely Intervention – Your care team reaches out when readings fall outside normal ranges, adjusting treatment before issues become serious
RPM isn’t new, but it’s experiencing explosive growth. Medicare started covering remote patient monitoring in 2018, and adoption has increased significantly each year since. The COVID-19 pandemic accelerated this shift, proving that effective healthcare doesn’t always require an in-person visit.
The numbers tell a compelling story. Nearly half of U.S. adults have high blood pressure, contributing to almost 700,000 deaths in 2023. More than 38 million Americans live with diabetes. COPD affects 16 million people and ranks as the third leading cause of death by disease in the United States. These chronic conditions require ongoing management—exactly what RPM was designed to support.
For patients frustrated by high costs, long waits, and the inconvenience of frequent clinic visits, RPM offers a better way. You stay comfortable at home while your healthcare team stays informed. Studies show this approach works: remote monitoring can lead to significantly lower blood pressure and cholesterol levels, reduced hospital readmissions, and better overall disease control.
RPM represents a fundamental shift from reactive to proactive healthcare. Instead of waiting until symptoms worsen, providers can spot problems early and adjust treatment plans before you end up in the emergency room. This matters for your health—and your wallet.
What is Remote Patient Monitoring and How Does It Work?
At its heart, remote patient monitoring (RPM) is a digital health solution that captures and records patient physiologic data outside of a traditional healthcare environment. We use RPM to empower both patients and providers to better manage acute and chronic conditions by collecting and sharing health information. This means instead of relying solely on periodic in-office visits, we can continuously track vital health metrics, gaining a more complete picture of a patient’s health status day-to-day.
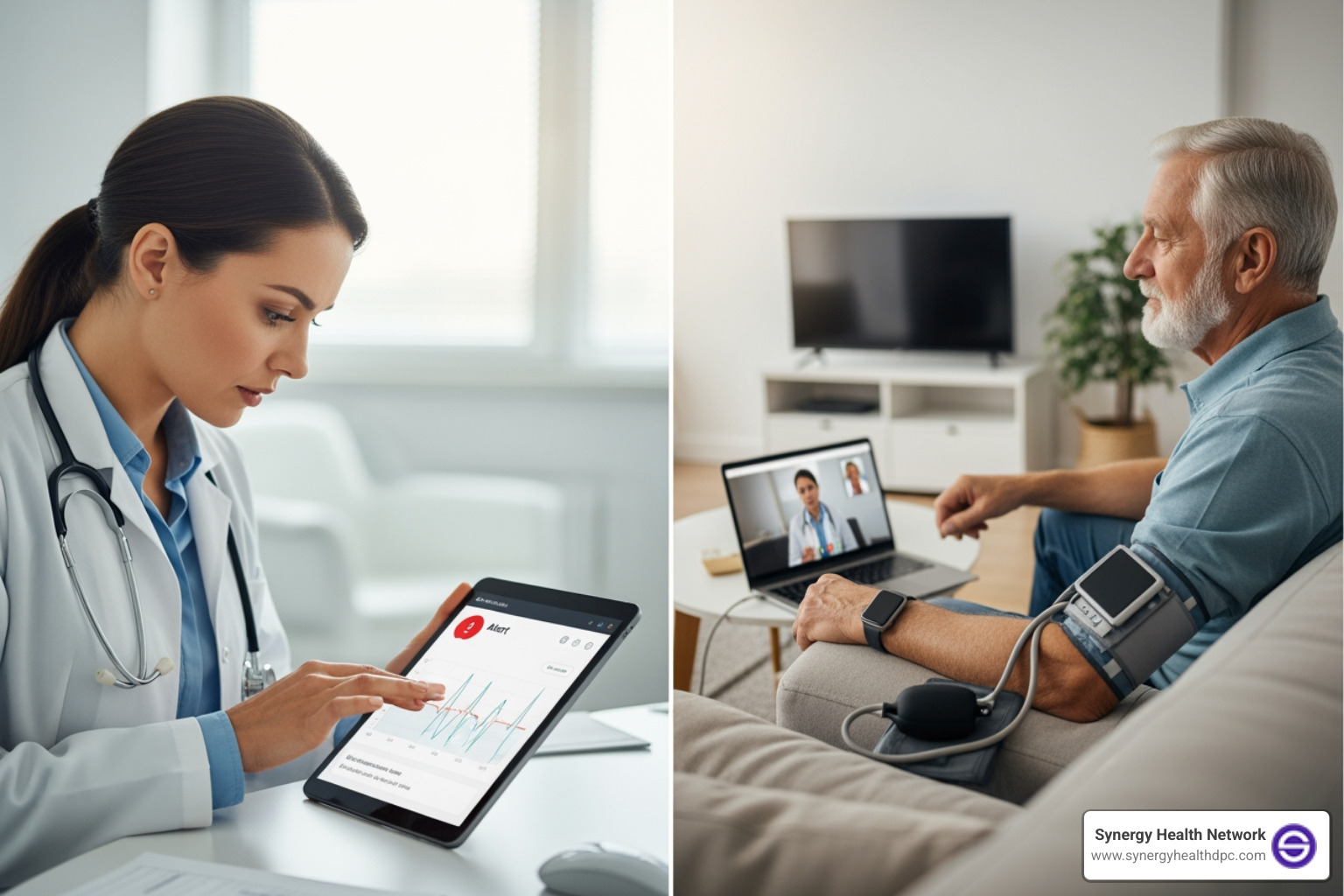
Think of it as having a healthcare safety net right in your home. Patients use easy-to-operate devices to measure things like blood pressure, blood glucose, oxygen levels, or weight. This data is then automatically and securely sent to their healthcare team. Our providers review this information, looking for trends or sudden changes that might indicate a worsening condition or a need for intervention. This proactive approach allows us to address potential problems early, often before they become serious enough to warrant an emergency room visit or hospitalization. It’s a fundamental shift towards more personalized, continuous, and responsive care.
The Core Components of an RPM System
A robust remote patient monitoring system isn’t just one device; it’s a carefully orchestrated combination of technology and human expertise. We see it built upon several pillars:
- FDA-Approved Medical Devices: These are the frontline tools. Patients use devices like smart blood pressure cuffs, connected weight scales, pulse oximeters, and blood glucose meters at home. Critically, these devices must meet the FDA’s definition of a medical device and be capable of digitally uploading data. This ensures accuracy and reliability.
- Data Transmission Technology: Once data is collected, it needs to get to the healthcare provider. This typically happens automatically via cellular networks (often built right into the device, eliminating the need for a smartphone) or Bluetooth, which pairs with a patient’s smartphone or tablet. The goal is seamless, effortless transmission for the patient.
- Secure Software Platform: All that collected data needs a home. A secure, cloud-based software platform acts as the central hub, receiving, storing, and organizing patient data. This platform often includes dashboards for clinicians to easily view trends, set alerts for abnormal readings, and communicate with patients. It’s also crucial for this platform to be HIPAA-compliant, ensuring patient data privacy and security.
- Clinical Staff and Workflows: Technology is only as good as the people and processes behind it. Our RPM programs rely on dedicated clinical staff—nurses, medical assistants, and physicians—who monitor the incoming data, interpret it, and initiate interventions when necessary. We establish clear workflows for data review, patient communication, and escalation protocols to ensure timely and effective responses.

Empowering Patients Through Engagement and Self-Care
One of the most profound impacts of remote patient monitoring is its ability to empower patients. When we provide patients with devices that allow them to regularly monitor their own health metrics, we give them a tangible role in their care journey. This fosters a sense of accountability and increases health literacy. Patients begin to understand how their daily choices—diet, exercise, medication adherence—directly affect their readings.
This improved understanding translates into improved self-management skills. For instance, a diabetic patient seeing their glucose levels fluctuate after certain meals might adjust their diet, or a patient with hypertension might be more diligent about taking their medication when they see its impact on their blood pressure readings. This direct feedback loop is incredibly motivating.
RPM also leads to improved communication between patients and their care teams. Instead of waiting for an appointment to voice concerns, patients can feel more connected, knowing their data is being monitored. This can reduce anxiety and provide immense peace of mind, especially for those managing complex or chronic conditions. While some patients might face Descriptions of barriers to self-care by persons with comorbid chronic diseases, RPM often helps overcome these by providing structured support and accessible tools. It transforms healthcare from something that happens to you into something you actively participate in.
The Transformative Benefits of Remote Patient Monitoring
The adoption of remote patient monitoring is not just about convenience; it’s about fundamentally improving healthcare delivery and outcomes. We’ve seen how RPM can lead to a cascade of benefits for both patients and the broader healthcare system.
At a high level, RPM contributes to:
- Improved Patient Outcomes: By providing continuous data, we can detect subtle changes in a patient’s health status earlier, allowing for timely adjustments to treatment plans. This often prevents conditions from worsening.
- Reduced Hospitalizations: One of the most significant benefits is the ability to intervene before a crisis. Early detection of fluctuations in a patient’s health status enables clinicians to intervene before a hospital visit is needed, thus lightening the load on the healthcare system and reducing unplanned emergency hospital use.
- Lower Healthcare Costs: Fewer emergency room visits and hospitalizations directly translate to lower costs for patients, payers, and the healthcare system as a whole.
- Improved Care Coordination: RPM platforms facilitate seamless data sharing among various members of a patient’s care team, ensuring everyone is working with the most up-to-date information.
- Increased Access to Care: For patients in rural areas, those with mobility issues, or individuals with busy schedules, RPM removes geographical and logistical barriers to consistent monitoring.
- Data-Driven Decisions: The wealth of continuous data collected through RPM allows providers to make more informed, evidence-based decisions about a patient’s care plan.
Key Benefits for Patients
For patients, remote patient monitoring offers a liberating experience that puts them at the center of their health journey:
- Convenience and Comfort: Patients can monitor their health from the comfort and privacy of their own homes, eliminating the need for frequent, time-consuming trips to the clinic. This is especially valuable for those with chronic conditions or mobility challenges.
- Fewer Trips to the Clinic: Imagine avoiding traffic, parking, and waiting rooms. RPM reduces the burden of travel, freeing up patients’ time and energy.
- Timely Interventions: Knowing that their healthcare team is reviewing their data daily provides reassurance. If a reading is outside the normal range, they can expect a quick response, preventing minor issues from escalating.
- Better Understanding of Their Condition: Regular monitoring demystifies health conditions. Patients gain a clearer picture of how their body responds to medication, diet, and activity, leading to greater self-awareness.
- Active Role in Their Health: RPM transforms patients from passive recipients of care into active participants. This engagement can be incredibly empowering and lead to better adherence to treatment plans.
Key Benefits for Healthcare Providers
For healthcare providers, remote patient monitoring is a game-changer, allowing us to deliver higher quality care more efficiently:
- Real-Time Patient Insights: Instead of relying on snapshots of health data from office visits, we get a continuous stream of information. This allows us to see trends, understand daily fluctuations, and catch early warning signs.
- Proactive Intervention Capabilities: With real-time data and customizable alerts, our care teams can intervene proactively. This means we can adjust medication, provide coaching, or schedule an earlier appointment before a patient’s condition deteriorates significantly. This predictive power reduces the likelihood of acute episodes.
- Reduced Clinician Burnout: By streamlining data collection and automating alerts, RPM can help manage workload. Clinicians can focus their attention on patients who genuinely need it, rather than sifting through less critical information. This targeted approach improves efficiency and can reduce the emotional toll of reactive care.
- Increased Practice Efficiency: RPM allows us to optimize our time and resources. We can manage a larger panel of patients more effectively, and patients who are stable can be monitored remotely, freeing up in-office appointments for those who require hands-on care.
- New Revenue Streams: For practices, RPM services represent an opportunity to expand care offerings and generate new revenue, particularly with the expanding Medicare coverage and the increasing number of commercial payers recognizing the value of these services. This financial aspect supports the sustainability and growth of our programs.
RPM in Action: Applications Across Medical Specialties
The versatility of remote patient monitoring means it’s not confined to just one area of medicine. We are seeing its transformative power across a wide array of specialties, enhancing chronic care management, improving postoperative recovery, ensuring the well-being of the elderly, and safeguarding maternal and fetal health. RPM helps us deliver more specialized and responsive treatment plans for diverse patient needs.
Cardiology: Managing Heart Health from Home
Cardiovascular conditions are among the most common chronic diseases, making them a prime area for remote patient monitoring to shine.
- Hypertension Management: Nearly half of U.S. adults can be classified with high blood pressure, and hypertension was a primary or contributing cause of nearly 700,000 deaths in 2023. We use RPM devices such as a blood pressure monitor to continuously track readings. This allows us to advise patients on lifestyle changes and adjust blood pressure medications with precision, leading to significantly lower blood pressure and cholesterol levels. The CDC provides more facts and statistics on the prevalence and impact of hypertension.
- Congestive Heart Failure (CHF) Monitoring: For the nearly 5 million Americans living with CHF, daily weight monitoring using a connected scale is critical. Cardiologists receive alerts when cardiac decompensation occurs, permitting fast action that helps improve the patient’s condition and decrease the need for hospitalization or urgent care. Patients can gain 10 pounds of ‘extra’ fluid weight before showing any symptoms besides increased weight, making continuous monitoring invaluable.
- Post-cardiac Event Care: After a heart attack or surgery, RPM can help monitor recovery, ensuring patients adhere to medication and rehabilitation protocols, and promptly identifying any complications.
Pulmonology: Breathing Easier with RPM
Respiratory conditions often require careful, ongoing management, and remote patient monitoring provides crucial visibility into a patient’s lung health.
- COPD Management: Chronic obstructive pulmonary disease (COPD) is the third leading cause of death by disease in the United States, affecting almost 16 million Americans according to the Center for Disease Control and Prevention (CDC). While incurable, COPD is manageable. We use a connected pulse oximeter to allow patients to report on their oxygen saturation levels and heart rate from home. This regular data helps pulmonologists perform effective and timely oversight, enabling interventions before severe exacerbations.
- Asthma Monitoring: More than 27 million U.S. adults—about 8%—have asthma. RPM devices, such as smart inhalers or spirometers, can track medication usage, lung function, and environmental triggers. This data helps patients and providers develop better management plans, reducing the frequency and severity of asthma attacks.
- Oxygen Saturation and Heart Rate: For various respiratory diseases or during viral outbreaks, monitoring oxygen saturation and heart rate from home is vital. RPM ensures these critical metrics are tracked consistently, providing early warning signs of distress.
Endocrinology: A New Era for Diabetes Management
Diabetes management is a complex, daily undertaking, and remote patient monitoring has revolutionized how we support patients with this condition.
- Blood Glucose Tracking: In 2021, more than 38 million Americans had diabetes. For many, regular blood sugar testing is essential. Patients increasingly receive remote support for their diabetes management via a blood glucose meter. When patients test their blood sugar, endocrinologists can review the data, evaluate the impact of diet and exercise, and track progress.
- HbA1c Level Control: Evidence shows that RPM is effective in controlling HbA1c levels in people with type 2 diabetes. This long-term indicator of blood sugar control can be significantly improved through consistent monitoring and timely adjustments to treatment.
- Medication Titration and Lifestyle Adjustments: RPM is ideal for medication titration, allowing clinicians to adjust insulin dosages or other diabetes medications based on real-time patient data. It also provides valuable insights for recommending lifestyle adjustments that contribute to better glucose control.
Specialized Applications: Postoperative, Elderly, and Maternal Care
Beyond chronic disease management, remote patient monitoring extends its reach to several other critical areas, demonstrating its broad applicability and impact.
- Post-surgery Recovery: Recovering from surgery can be a vulnerable time. RPM devices can track relevant postoperative health indicators such as heart rate, temperature, and frequency of movement. This allows patients to recover in the comfort of their homes while their care team monitors their progress, helping to avoid serious complications and detect issues like medication errors more effectively than standard care.
- Aging in Place (Elderly Care): For our elderly population, RPM offers a pathway to maintain independence and safety at home. Systems can include motion detectors, temperature sensors, and bed monitors that alert caregivers or emergency responders if unusual activity or a fall is detected. This continuous surveillance is invaluable for promoting safety and peace of mind for both the elderly and their families.
- High-Risk Pregnancies and Fetal Monitoring: Pregnancy, particularly high-risk cases, benefits immensely from RPM. Remote maternal and fetal monitoring systems, often utilizing smartphone apps, measure the fetus’s heart rate and response to uterine contractions. This enables care providers to remotely monitor their pregnant patients, allowing for informed decisions and timely interventions. This is especially crucial given that there are nearly 2 million stillbirths every year globally, with more than 40% occurring during labor—losses that could be avoided with improved quality of care and monitoring.
Implementing an RPM Program: A Guide for Providers
Implementing a successful remote patient monitoring program requires careful planning and execution. It’s not just about buying devices; it’s about integrating new technology and workflows into existing clinical practice while ensuring patient and staff buy-in. We’ve learned that a structured approach is key.
Patient Eligibility and Financial Considerations
Understanding patient eligibility and the financial landscape is crucial for any RPM program.
- Medicare Coverage: Medicare broadly covers remote patient monitoring (sometimes called remote physiologic monitoring) for the collection of any type of physiologic data using a wide range of devices, for chronic and acute conditions. To be eligible for RPM services under Medicare, a patient must:
- Have a chronic or acute condition that requires monitoring.
- Use an internet-connected device that meets the FDA’s definition of a medical device and digitally uploads data.
- Collect and transmit health data at least 16 days every 30 days.
Medicare started covering RPM in 2018, and we’ve seen the number of patients utilizing these services increase significantly each year since.
- CPT Codes and Reimbursement: Reimbursement for RPM services is typically tied to specific CPT (Current Procedural Terminology) codes. These codes cover aspects like the initial setup and patient education, the supply of the device, and the time spent by clinical staff reviewing and managing the patient’s data. Medicare generally pays for these three main components separately. It’s essential for providers to stay updated on the latest billing guidelines. We recommend subscribing to the CMS MLN Connects® newsletter for updates on Medicare coverage, billing, and payment. Beyond Medicare, an increasing number of commercial payers are also covering RPM services, reflecting the growing recognition of its value.
Overcoming Implementation Challenges
While the benefits are clear, we acknowledge that implementing remote patient monitoring comes with its own set of challenges. Addressing these proactively is vital for success:
- Patient Adherence and Technology Literacy: Not all patients are equally comfortable with new technology. We need to provide thorough, patient-centered training and support to ensure they understand how to use their devices and transmit data consistently. Some patients may also need motivational interviewing to sustain engagement.
- Data Overload for Clinicians: RPM generates a significant amount of data. Without proper systems and workflows, this can quickly become overwhelming for clinicians. The key is to implement intelligent platforms that filter data, highlight critical alerts, and present information in an easily digestible format.
- Interoperability with EHRs: Integrating RPM data seamlessly into existing Electronic Health Record (EHR) systems can be complex. We strive for solutions that allow for smooth data flow, avoiding manual entry and ensuring all patient information is centralized.
- Data Privacy and Security (HIPAA): Transmitting sensitive health data wirelessly raises critical privacy and security concerns. We ensure that all RPM platforms and processes are fully HIPAA-compliant, using robust encryption and secure access protocols to protect patient information.
Getting Started with a Remote Patient Monitoring Program
For healthcare providers looking to accept remote patient monitoring, we recommend a systematic approach:
- Identify Target Patient Population: Start by pinpointing specific patient groups who would benefit most from RPM. This could be patients with uncontrolled hypertension, diabetes, CHF, or those requiring postoperative monitoring.
- Choose an RPM Partner/Platform: Select a technology partner whose platform is user-friendly for both patients and clinicians, offers FDA-approved devices, ensures data security, and provides excellent customer support.
- Develop Clinical Workflows: Design clear, efficient workflows for how data will be monitored, who will respond to alerts, how often patients will be contacted, and how RPM data will be integrated into the patient’s overall care plan and EHR.
- Train Staff and Educate Patients: Provide comprehensive training for your clinical team on the RPM platform and new workflows. Equally important, thoroughly educate patients on device usage, data transmission, and what to expect from the program, including emergency protocols.
- Launch and Monitor the Program: Begin with a pilot program, track key metrics, gather feedback from both staff and patients, and continuously refine your processes. Iterative improvement is key to scaling successfully.
Frequently Asked Questions about Remote Patient Monitoring
What is the difference between Remote Patient Monitoring (RPM) and telehealth?
Telehealth is a broad umbrella term that encompasses all remote healthcare services delivered through technology. This includes video consultations (telemedicine), e-visits, remote physical therapy, and even certain types of patient education delivered digitally. Remote patient monitoring is a specific type of telehealth focused on the collection and monitoring of physiologic data from a distance. While RPM is a component of telehealth, not all telehealth involves RPM. For example, a video call with your doctor is telehealth, but it’s not RPM unless you’re also transmitting health data from a connected device.
What is the difference between Remote Patient Monitoring (RPM) and Continuous Glucose Monitoring (CGM)?
Remote patient monitoring is a comprehensive approach that can track a wide range of physiologic data, including blood pressure, weight, oxygen saturation, and, yes, glucose levels. It’s used for various acute and chronic conditions. Continuous Glucose Monitoring (CGM), on the other hand, is a specific technology primarily used for diabetes management. CGM continuously tracks glucose levels throughout the day and night, providing real-time insights that traditional fingerstick tests can miss. While CGM devices often transmit data wirelessly to a patient’s smartphone or a remote system, making them a form of remote monitoring, CGM itself is a specialized device and not the entire RPM program. A CGM system can be a crucial component of a broader RPM program for a diabetic patient.
What kind of devices are used in RPM?
A variety of medical-grade devices are used in remote patient monitoring, all designed to be easy for patients to use at home and capable of digital data transmission. Common examples include:
- Blood Pressure Cuffs: For monitoring hypertension and other cardiovascular conditions.
- Weight Scales: Essential for managing conditions like congestive heart failure and obesity.
- Pulse Oximeters: Used to measure oxygen saturation levels and heart rate, particularly for respiratory conditions like COPD or during acute illnesses.
- Blood Glucose Meters: For patients with diabetes to track their blood sugar levels.
- Thermometers: For monitoring body temperature, especially during infections or postoperative recovery.
- ECG Monitors: Portable devices that can record heart activity to detect arrhythmias.
All these devices must meet FDA standards for medical devices to ensure accuracy and reliability.
Conclusion
Remote patient monitoring is more than just a technological trend; it’s a fundamental shift in how we approach healthcare. By leveraging connected devices and intelligent platforms, we are moving towards a future of proactive, personalized care that keeps patients healthier, more engaged, and more comfortable in their own homes. The benefits are clear: improved health outcomes, reduced hospitalizations, and a more efficient healthcare system for everyone.
At Synergy Health DPC, we believe in embracing innovative virtual care solutions that put your health first. Our model is built on providing unlimited virtual visits, 24/7 provider access, and personalized treatment with no copays, all for a single monthly fee. Remote patient monitoring perfectly complements this philosophy, allowing us to stay connected to your health journey and intervene precisely when needed.
As healthcare continues to evolve, RPM will play an increasingly vital role in ensuring that quality care is accessible, effective, and custom to individual needs. We are excited to be at the forefront of this change, helping our patients live their healthiest lives.
Learn how virtual urgent care can complement your health management.